Dispatches From the COVID-19 Frontlines
Nephrologist Joris Rotmans, Netherlands
Dispatches From the COVID-19 Frontlines
Nephrologist Mariles Reinders, Netherlands
Conversation with Two US Nephrologists on the COVID-19 Frontlines
Dr. Summit Mohan & Dr. Raghu Durvasula

Conversation with Dr. Usman Galadima, ISN Fellow, on a Nigerian national TV in Abuja on COVID-19
Dr. Usman Galadima
Dispatches from the Young Nephrologists’ Frontlines
Three months ago, the coronavirus seemed to be a distant alert, but it quickly arrived in Brazil and had a different intensity among the macro-regions. Metropoles such as São Paulo and Rio de Janeiro were the first to experience the impact of the pandemic. Porto Velho, the capital of the State of Rondônia, in Western Amazonia, was not exempt from the pandemic route. It is a city with almost 550,000 inhabitants.
New ICUs were progressively opened, health teams were trained, schools were closed, and commerce was reduced. But all efforts failed to contain the increase in sick patients with severe evolution, especially in obese and male patients.
Within weeks, all ICU beds were occupied. Nephrology was essential; a large proportion of patients, especially those on mechanical ventilation, needed dialysis.
The challenges gradually appeared: doctors and staff fell ill, supplies were lacking or cost significantly more, and hours of overtime began.
In dialysis clinics, disease transmission was high among patients and staff, and even though these patients received all the necessary intensive support, death was almost inevitable. It felt like we were in quicksand.
In the midst of so much sadness and tiredness, something caught our attention: the strong teamwork. We were surprised by the feeling of solidarity and partnership. Those involved in the nephrology and intensive care sectors were fully focused on making the whole process feasible. That gave us the extra strength needed to continue day after day.
Today, we are still in the middle of the hurricane, but we continue to be united, and we are sure that all this will pass soon. We will look back and be proud to have faced the COVID pandemic as nephrologists on the front line.
Since it is a novel disease, the modus operandi of COVID-19 management has needed to change over time in Bangladesh in line with our country’s needs and national guidelines of COVID-19 management.
Early in March 2020, when a handful of corona positive cases were detected, we focused mainly on prevention, educational programs for health workers regarding the management of the new disease, and updated training on personal protection.
For all patients coming to the hospital, including patients on dialysis, there is triage for preliminary screening. When patients present with suspected COVID-like symptoms, they are managed in separate zones. Direct OPD consultation is limited, and a telemedicine service has been developed to prevent disease spread from the OPD.
Special precaution was taken for the Dialysis Unit as a potential portal of infection. We’ve also educated the patients about preventive measures, symptoms of COVID-19, and advised them to seek help through telemedicine rather than coming directly to the Dialysis Unit. Throughout this period, we emphasize maintaining regular dialysis as volume overload may erroneously mimic the COVID infection. For emergency dialysis, we prefer Femoral Venous Catheterization instead of the Internal Jugular route. The use of complete PPE is mandatory during procedures.
Initially, COVID hospitals were designated in the country. When community transmission occurred on a large scale, the Health Authority decided to treat both COVID and non-COVID patients in all hospitals. We divided our hospital into COVID, non-COVID, and suspected COVID zones. Eventually, we started doing RT-PCR in our hospital. Currently, we are providing renal consultation, dialysis of COVID patients in the Critical Care Area, and have built a negative pressure isolation chamber for COVID positive dialysis patients. In my experience, treating COVID and non-COVID patients in the same center is still challenging, especially when RT-PCR is not readily available, and waiting times to get test results are long. Further, a robust and integrated infection control strategy, surveillance, and logistical support are needed.
Sadly, many patients hide their actual history, thus posing a greater threat to physicians. As large-scale community transmission occurs, patients are now presenting with different symptoms and test COVID positive incidentally during screening. Sometimes highly suspected cases are found as COVID negative in an initial test, but subsequent test results prove positive. Therefore, I always emphasize wearing a proper N95 or equivalent mask/respirator to my fellow colleagues whenever they come into contact with any patient.
Bangladesh has unfortunately observed a high rate of physician deaths due to COVID-19 within a very short period. Therefore, priority measures need to be taken to find out the exact causes of their demise.
Ever since we recorded our first two cases in Ghana on March 12, 2020, our COVID-19 cases have been rising. According to the Ghana Health Services, as of June 28, we had 17,351 cases: 4,245 active cases, 12,994 recovered or discharged, and 112 deaths. We have tested 288,465 people so far, which is the third-highest rate in Africa after South Africa and Morocco.
There have been some government interventions to contain the COVID-19 virus. The first major intervention was the closure of the borders on March 22, 10 days after we recorded our first cases. Then a partial lockdown was declared in the epicenters from March 30 for three weeks to carry out aggressive contact tracing and minimize the spread of the virus. Although cases were still rising, the partial lockdown had to be lifted by the government due to social and economic hardships.
Restrictions on public and social gatherings were still in place, but these also eased as the president announced the lifting of the ban on religious activities with strict measures to govern services, such as a maximum duration of one-hour for up to 100 people and strict following of all safety protocols. The president encouraged social distancing and made the wearing of facemasks in public mandatory in Ghana, punishable by law, as additional restrictions were eased.
There is now a gradual effort to re-open schools. Final-year students in tertiary and secondary high schools resumed on June 15 to prepare their final examinations. On June 29, Junior High School final-year students resumed classes. School heads are expected to ensure all safety protocols.
My worry as a healthcare professional is the fact that there may be an escalation of cases, which might overwhelm our health institutions. Staff in most hospitals are decreasing as about 100 doctors have currently been infected with COVID-19. We have recorded two deaths from COVID-19, a Medical Director, and the renowned Nephrologist and Rector of the Ghana College of Physicians and Surgeons, Prof. Jacob Plange-Rhule. The Health Minister in Ghana has also tested positive for COVID-19.
With some people blatantly disregarding safety protocols after the easing of restrictions, and decreasing staff strength with inadequate provision of PPEs, I fear there will be more deaths from COVID-19 as cases increase. There is a possibility of an increase in the number of non-COVID-19-related deaths as a result of the shortage of staff due to self-isolation when exposed or overwhelmed with COVID-19 management, as written in an article I published, which was reported as a news item.
Unfortunately, this year is an election year for Ghana, and it’s worrying that political activities are going on with people flouting safety protocols of social distancing and wearing face masks. With the upcoming voters’ registration exercise starting on June 30 leading up to the elections in December 2020, we can only hope that these do not worsen the already increasing cases of COVID-19 in Ghana.
As for most people around the world, I think few of us here could imagine the impact this outbreak would have, not just on our health system, but on the daily rhythm and comforts of our lives. Australia has, thus far, been spared from the large-scale infection and death rates seen in other places around the world. Nevertheless, we continue to be in a state of partial lockdown and our health structures and operations are only just contemplating a return to the traditional models of care.
In our hospital, wards were geographically re-structured to minimize staff traffic and to accommodate a burden of COVID-infected patients that has yet to come. Our outpatient clinics changed almost completely to phone consultations, forcing us to audit and triage our lists to select only the very few that required in-person attention.
I found this especially difficult working with a predominantly home dialysis and transition group of patients for whom close follow-up, planning, training, and importantly, reassurance and support are key. Despite these challenges, I have been overwhelmed by our patients’ gratitude and empathy and the dedication and steadfastness of our staff. As a pregnant clinician through these times, I have felt the protection and concern of my colleagues for my well-being and the enormous solidarity that exists among our medical community.
I think one of the most important aspects of the COVID-19 pandemic has been the psychological impact on nephrologists and other healthcare workers due to lack of organization and clear directives from health care authorities in terms of outpatient dialysis operations, the organization of a referral center for COVID-19 positive patients, the lack of PPE, and false information (unreliable sources from social media). All of these issues have caused them to feel anxious and distressed.
The workload has dramatically increased especially for young nephrologists and fellows, and some of them have started to show early signs of burnout. This is partly because the Bolivian Minister of Health has withdrawn personnel over 60 years old from hospitals and health care centers if they have chronic diseases such as diabetes and hypertension, and any pregnant personnel. This has had a significant impact on the physicians and other health care workers who remain working at hospitals and health care centers in Bolivia.
We have to take practical steps to prepare our nephrologists, fellows, and nurses to give the best care possible for patients with kidney disease during the COVID-19 pandemic and to prevent transmission by giving them online lectures on COVID-19 and kidney disease, create infographics in Spanish of different practical issues like how to educate patients, and how to organize hemodialysis units.
Fortunately, so far we haven’t had any COVID-19 positive patients with ESKD on chronic dialysis; I think this could be explained in part by education campaigns – launched for patients and their families, social distancing, and the early lockdown established by the national government just 2 weeks after the first 2 cases of COVID-19 were reported.
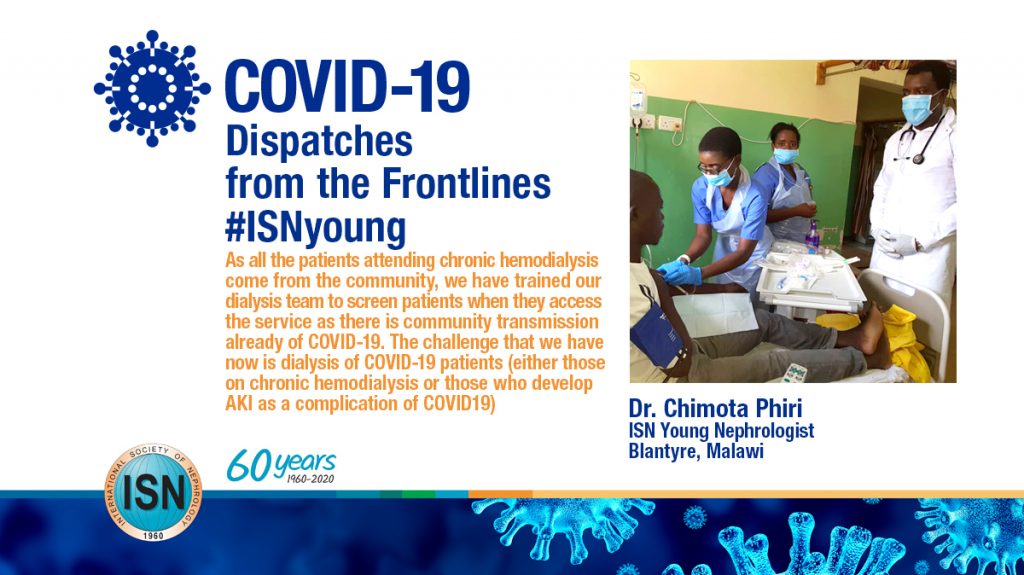
Malawi has not been spared from the COVID-19 pandemic. So far we have recorded 33 confirmed cases with 3 deaths, but the actual number of infections may be underestimated as testing is not happening on a large scale. As a response to COVID-19, most of the clinics have been scaled down including general nephrology and hypertension clinics but patients on immunosuppression will be seen as per schedule.
With the government issuing restrictions on public gatherings and transport, the public transport fee has gone up rendering it difficult for health workers and patients to get to and from the hospital. Recently, government health workers went on strike to demand availability of personal protective equipment (PPE) and help to mitigate rising transport costs. This had an impact on patients with kidney disease who could not be properly cared for in the ward or access renal services appropriately. Luckily, this has been sorted out swiftly by the government and now services have returned to normal.
As all the patients attending chronic hemodialysis come from the community, we have trained our dialysis team to screen patients when they access the service as there is community transmission already of COVID-19. The challenge that we have now is dialysis of COVID-19 patients (either those on chronic hemodialysis or those who develop acute kidney injury as a complication of COVID19). Ideally, we should have a portable dialysis machine that could be moved around for patients in isolation who may benefit from dialysis.
Malawi is a landlocked country and is dependent on supplies being transported from other countries, like South Africa. Hence, lockdown measures and limitations on movement might negatively impact dialysis supplies. We are uncertain of how long the lockdown measures in neighboring countries will last so that we can replenish our supplies.