March 2024 Edition

Current science in acute kidney injury (AKI) is rapidly evolving, with research focusing on early detection, mechanisms of injury, and novel treatment approaches. Recent studies published in Kidney International® and Kidney International Reports® shed light on various aspects of AKI, offering insights into its pathophysiology, risk factors, and clinical management strategies. These papers contribute to advancing our understanding of AKI and improving patient outcomes in this critical condition.
KIDNEY INTERNATIONAL ARTICLES |
A Comprehensive Description of Kidney Disease Progression After Acute Kidney Injury From a Prospective, Parallel-Group Cohort Study

A prospective study delineating kidney disease progression.
Long-term and future adverse effects involving kidney and cardiovascular health are part and parcel of acute kidney injury (AKI) and increase morbidity and mortality. There have been limited prospective studies in this field. It is refreshing to see a prospective study for AKI that combats confounding and ascertainment bias.
A prior US-based large prospective study confirmed an increased risk of chronic kidney disease (CKD) after AKI. That study, however, involved more critical patients compared to this one. Although the Acute Kidney Injury Risk in Derby (ARID) study is similar, it includes patients in the general ward.
This study also shows that albuminuria must be accounted for when discussing advancing kidney disease and progression to CKD. AKI has been linked to serious long-term problems for patients. More planning and research are required to establish meaningful interventions, follow-up, and post-discharge care in the affected patient population.
Association of HIV and Viral Suppression Status With Hospital Acute Kidney Injury in the Era of Antiretroviral Therapy
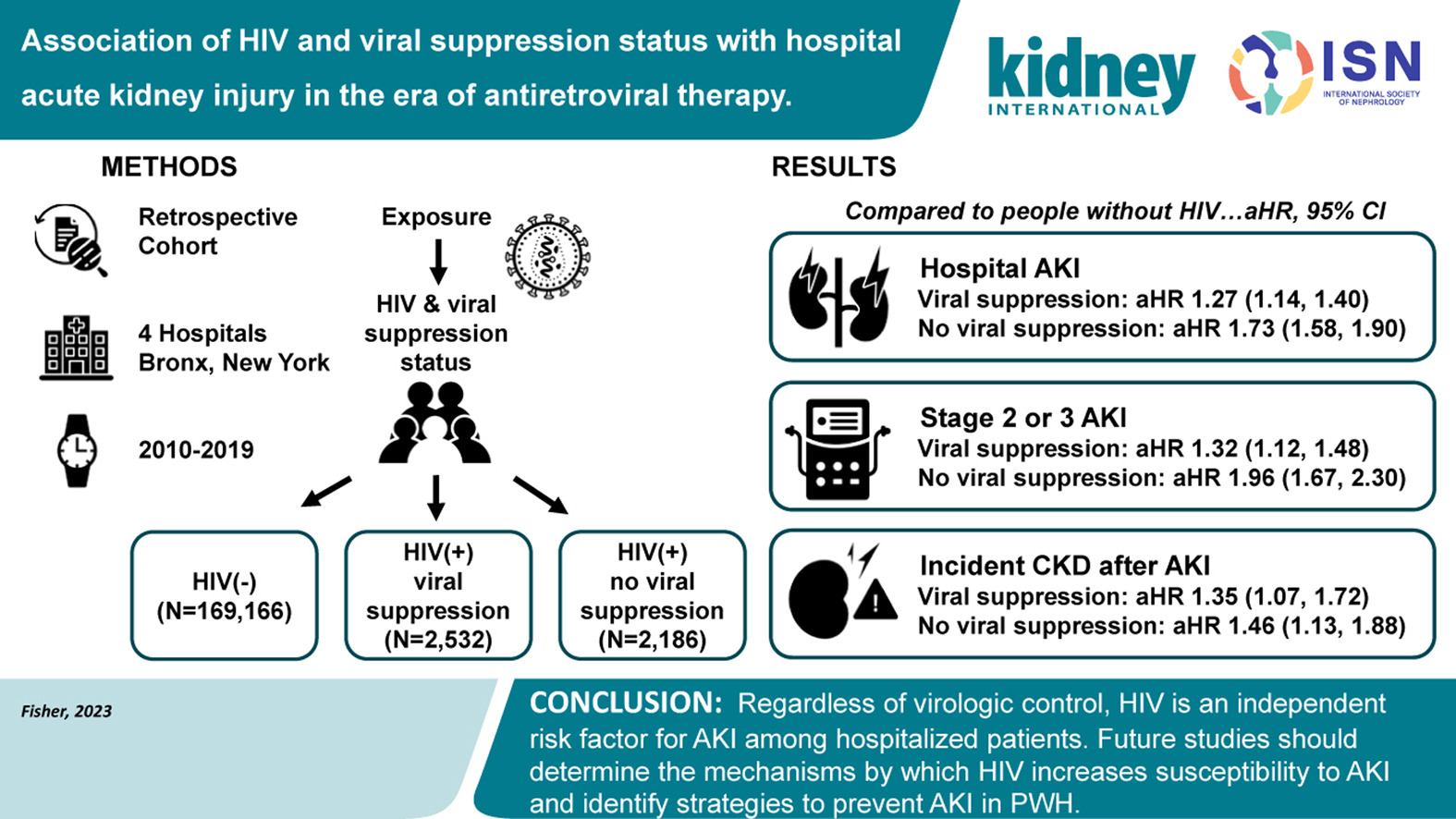
This retrospective observational cohort study analyzed data from a large New York City health system between 2010 and 2019. The authors compared the incidence of hospital acute kidney injury (AKI), stage 2 or 3 AKI, and incident chronic kidney disease (CKD) following AKI among patients with a diagnosis of HIV infection (both with and without viral suppression) and patients without HIV.
The study included 172,884 hospitalized patients, of whom 4718 had HIV and 2532 were virally suppressed. The incidence of hospital AKI, stage 2 or 3 AKI, and incident CKD were higher among those with HIV than without. Among those with HIV and no viral suppression, the outcomes were less favorable than among those with viral suppression. The study highlights that regardless of virologic control, HIV is an independent risk factor for AKI among hospitalized patients.
Microbiome Modulation After Severe Acute Kidney Injury Accelerates Functional Recovery and Decreases Kidney Fibrosis
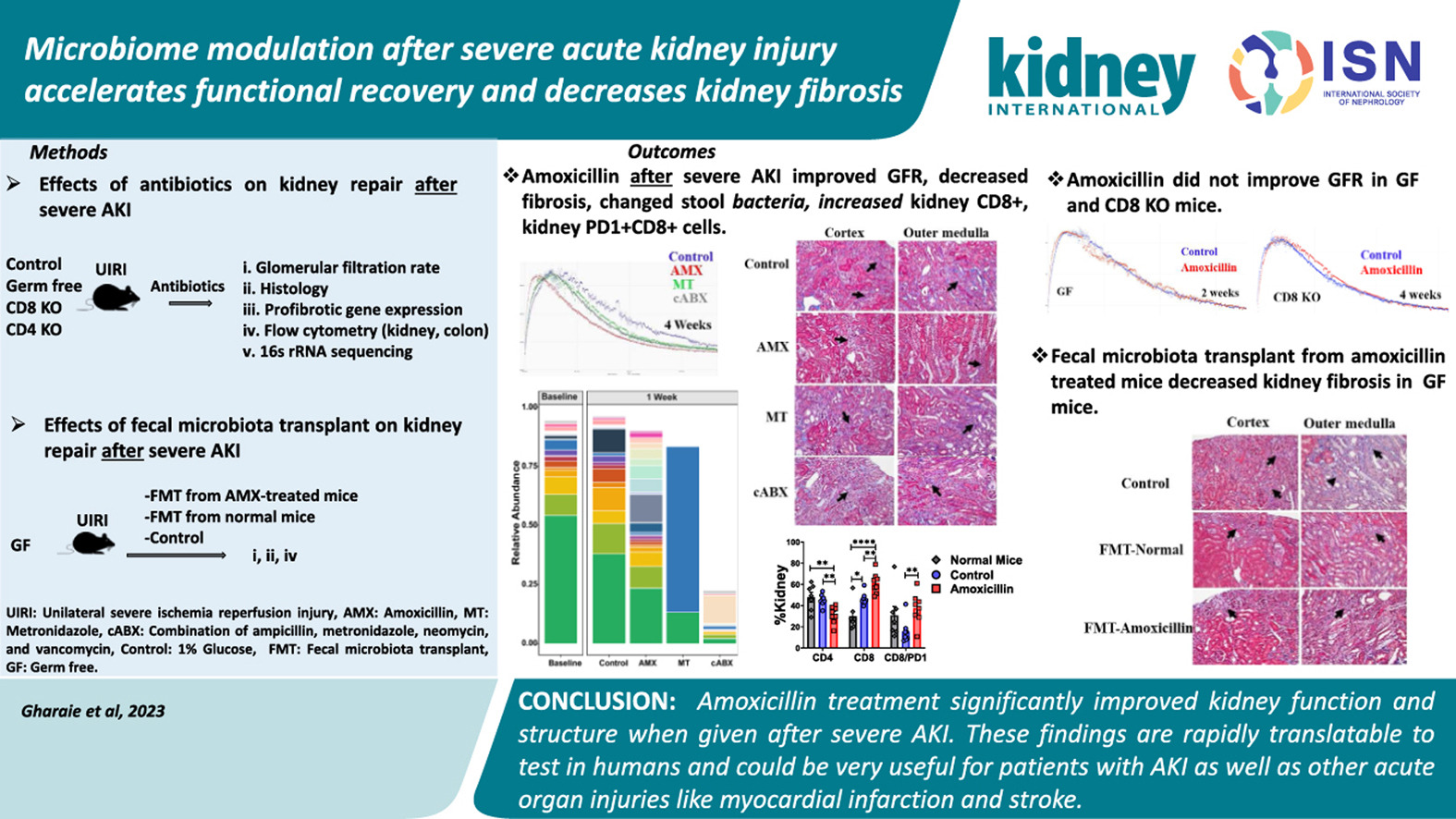
The gut microbiota, a complex community of microorganisms in the digestive system, plays a crucial role in overall health, including kidney function. The interaction between gut microbiota and kidneys is a key aspect of metabolic and immune regulation. Changes in gut microbiota composition can impact renal health, influencing processes such as inflammation, immune response, and toxin clearance. Dysbiosis, an imbalance in gut microbiota, has been linked to various kidney diseases, suggesting that targeting gut microbiota could offer therapeutic benefits for kidney-related conditions. In a recent study, targeting gut microbiota showed promise in not only preventing acute kidney injury (AKI) but also in enhancing recovery and preventing fibrosis. The study focused on the effects of modifying gut microbiota using antibiotics, specifically amoxicillin, in mice after severe ischemic kidney injury. The treatment led to significant improvements, including increased glomerular filtration rate, reduced kidney fibrosis, and lowered expression of profibrotic genes. Amoxicillin altered the gut microbiota composition, increasing certain bacterial species while decreasing others, significantly influencing various immune cells. Notably, it reduced kidney cluster of differentiation 4 double negative T cells (CD4+ DN T), interleukin 17 cluster of differentiation 4 double negative T cells (IL-17 CD4+ DN T), and tumor necrosis factor-α double negative T cells while increasing cluster of differentiation 8 double negative T cells (CD8+ DN T) and programmed cell death protein, cluster of differentiation 8 double negative T cells (PD1 CD8+ DN T).
The protective effects of amoxicillin were dependent on the microbiome and CD8+ DN T lymphocytes, as shown by its ineffectiveness in germ-free or CD8-deficient mice.
Interestingly, fecal microbiota transplantation from amoxicillin-treated to germ-free mice also reduced kidney fibrosis. However, amoxicillin pre-treatment did not protect against cisplatin-induced AKI.
The study highlights the potential of using antibiotics like amoxicillin post-ischemic AKI to accelerate kidney recovery and prevent chronic kidney disease progression, underlining a novel therapeutic approach involving gut microbiota modification.
Downregulation of G Protein-coupled Receptor Kinase 4 Protects Against Kidney Ischemia-Reperfusion Injury
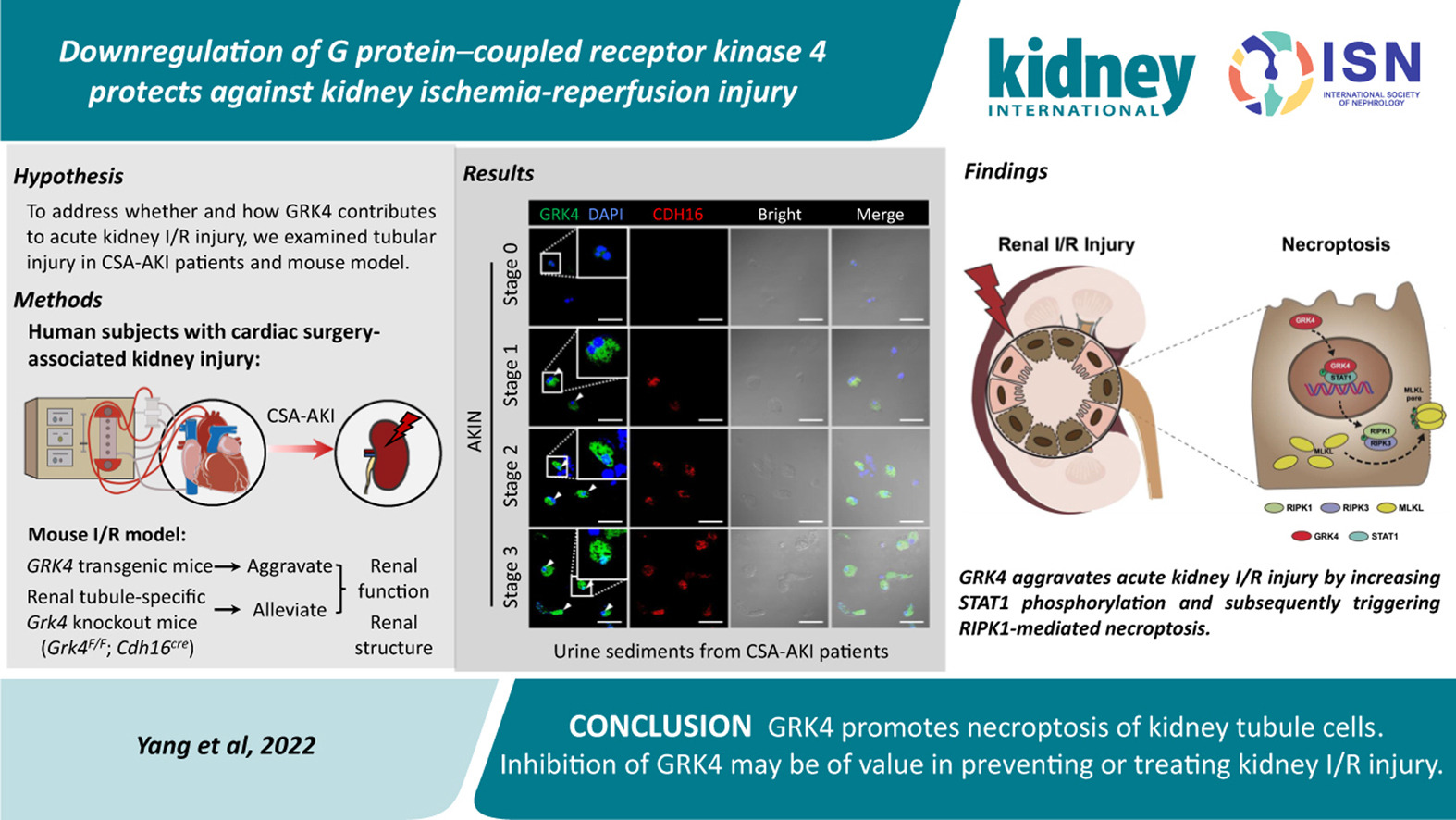
One important mechanism in renal ischemia/reperfusion (I/R)-induced acute tubular necrosis is necroptosis. The current investigation determined the function of G protein-coupled receptor kinase 4 (GRK4) in tubule cell necroptosis. Protective effects were achieved by GRK4 deficiency or downregulation using drug delivery based on nanoparticles. These results imply that GRK4 is a potential therapeutic target and regulates the degree of kidney I/R injury.
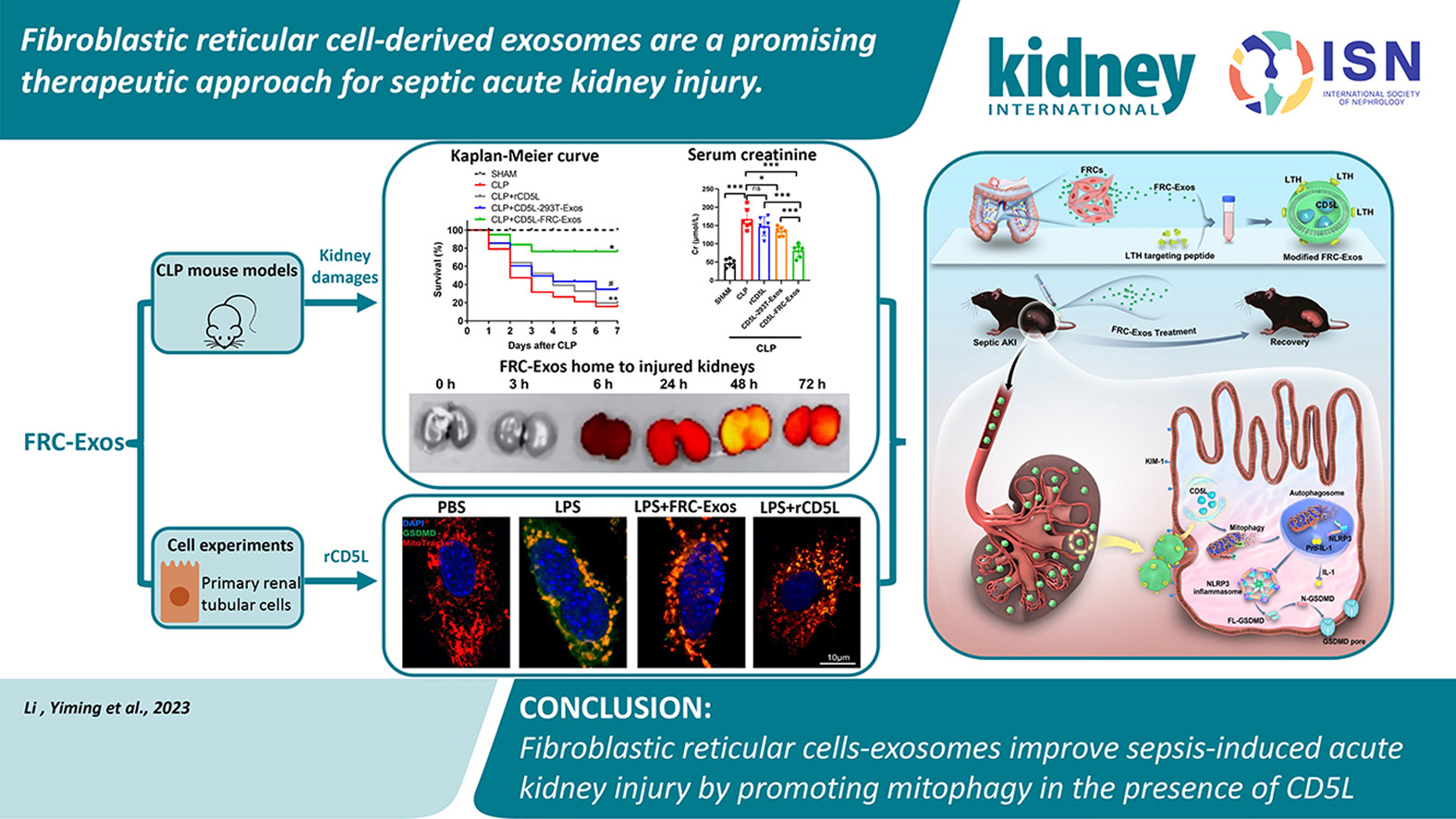
Sepsis-induced acute kidney injury (S-AKI) is a critical and often fatal complication arising from sepsis, a severe and body-wide response to infection. This condition significantly impacts kidney function, leading to a high mortality rate among affected patients. Despite its seriousness, there are currently no specific medications available to effectively treat S-AKI. This lack of targeted therapies presents a significant challenge in clinical settings, emphasizing the urgent need for research and development in this area. The development of effective treatments for S-AKI is crucial to reduce mortality rates and improve outcomes for patients suffering from this severe complication of sepsis.
The study explores a novel treatment for S-AKI, a condition with high mortality and limited treatment options. It focuses on the therapeutic potential of fibroblastic reticular cell-derived exosomes (FRC-Exos). The research demonstrates that FRC-Exos, especially when modified to contain higher levels of the protein CD5L, effectively target and improve kidney function in a mouse model of sepsis. This improvement is achieved by mechanisms such as promoting mitophagy and inhibiting inflammasome activation in kidney cells.
The study reveals that these modified exosomes, when compared to recombinant CD5L, show enhanced binding specificity and efficacy in mitigating kidney damage and improving survival rates in sepsis. This research opens up new possibilities for developing targeted therapies for S-AKI, addressing a critical gap in current treatment options.
KIDNEY INTERNATIONAL REPORTS ARTICLE |
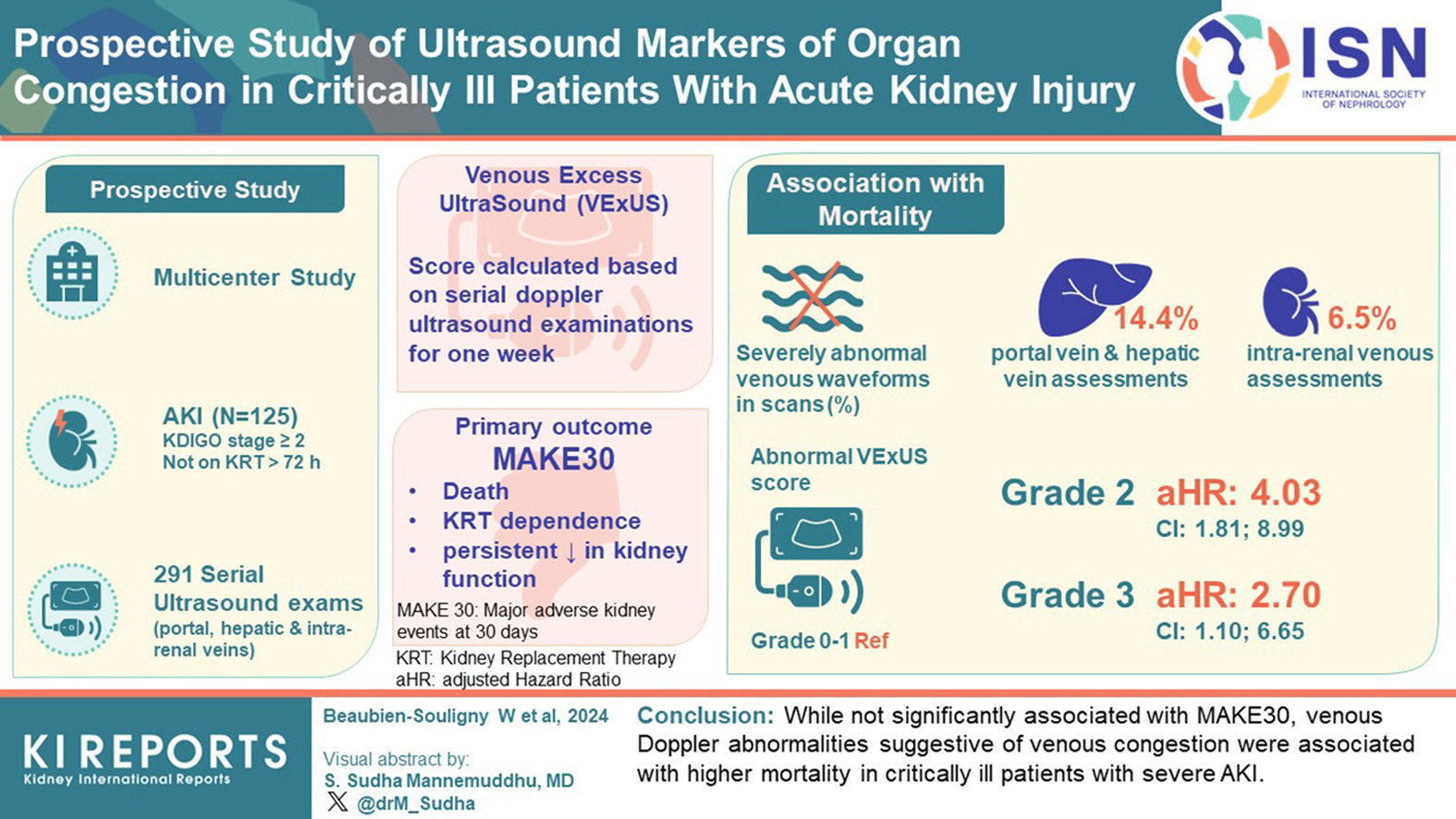
This prospective, multi-center study of patients with severe AKI investigated the utility of Doppler ultrasound to identify adverse outcomes. Venous Doppler abnormalies were not significantly associated with MAKE30 but demonstrated evidence of increased mortality. Critical patients with cardiovascular involvement were found to have significant venous Doppler markers and congestive changes compared to counterparts with sepsis and other medical diagnoses. The VExUS score was also associated with mortaility, suggesting its promise as a measurement tool.
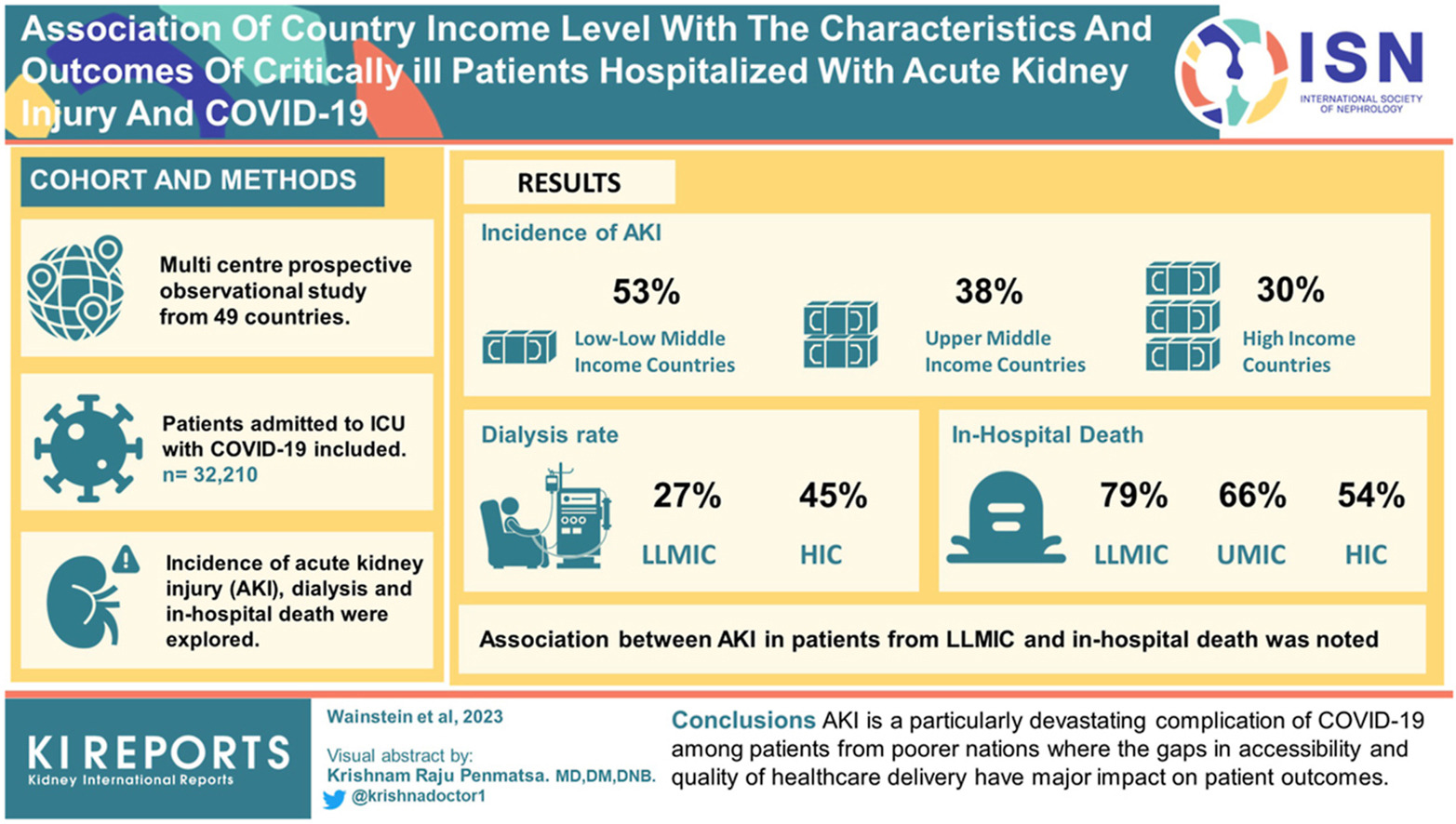
This multi-center prospective observational study examined the relationship between COVID-19-related acute kidney injury (AKI) characteristics and World Bank country income classifications. The study recruited 32,120 adults from 49 countries with laboratory-confirmed SARS-CoV-2 infection requiring hospital admission and intensive care from January 30, 2020, to September 1, 2022. The countries included 8 low- and low-middle-income countries (LLMIC), 11 upper-middle-income countries (UMIC), and 30 high-income countries (HIC).
AKI incidence was highest in patients in LLMIC, followed by UMIC and HIC, whereas dialysis rates were lowest among patients with AKI from LLMIC and highest among those from HIC. Patients with AKI in LLMIC had the most significant proportion of community-acquired AKI and the highest rate of in-hospital death. The association between AKI, being from an LLMIC, and in-hospital death persisted even after adjusting for disease severity. The results suggest poorer nations have more COVID-19-related AKI and worse outcomes.
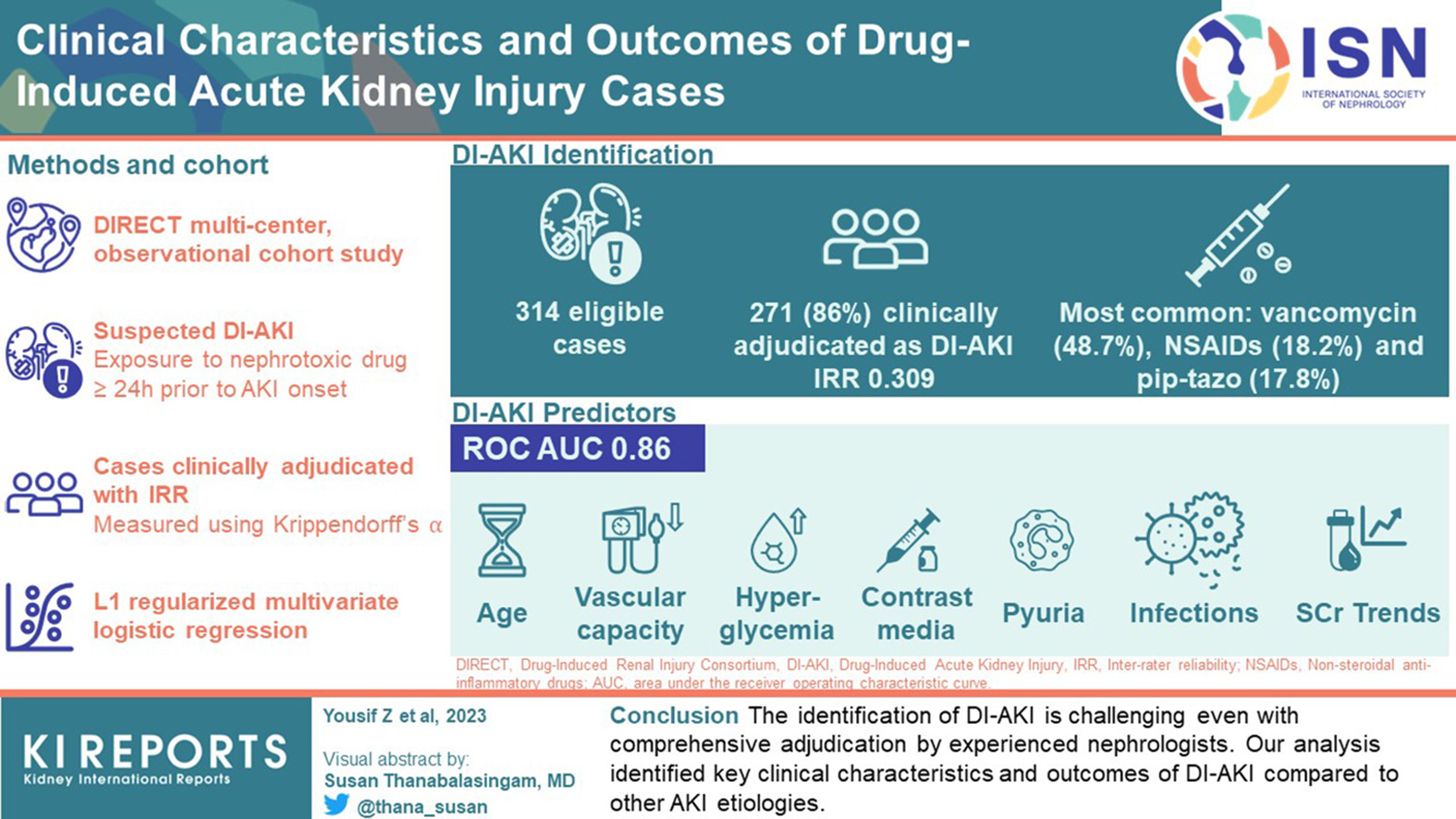
Drug-induced acute kidney damage (DI-AKI) is a common adverse effect. Competing etiologies, clinical variability among individuals and a lack of precise diagnostic techniques pose challenges in identifying DI-AKI. Our study seeks to describe the clinical features and prognostic indicators of DI-AKI. The study comprised patients who met the criteria for drug-induced kidney damage as recognized by several scales.
A multivariate logistic regression model was built, and its performance was evaluated using the area under the receiver operating characteristic curve (ROC AUC). The multivariable model found age, vascular capacity, hyperglycemia, infections, pyuria, serum creatinine (SCr) trends, and contrast media as important predictors of DI-AKI with high performance (ROC AUC 0.86). DI-AKI is difficult to identify. This study’s research highlighted critical clinical characteristics and outcomes of DI-AKI compared to other AKI etiologies.
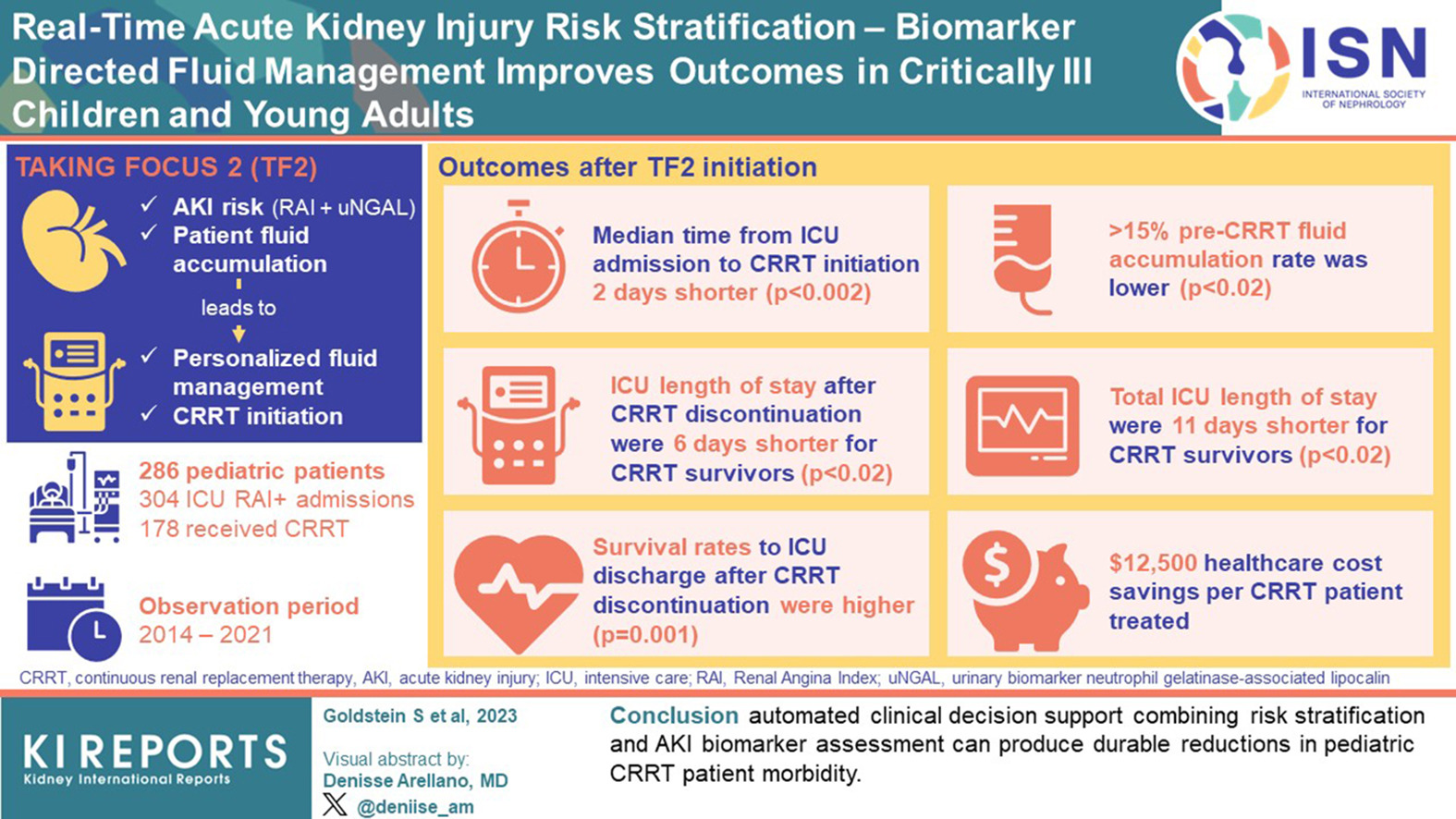
Many tools and biomarkers have been used to assess acute kidney injury (AKI) risk and help guide treatment. In this trial performed by Goldstein and cols., they used NGAL and fluid overload combination (TAKING FOCUS 2, TF2) to personalize fluid management and continuous renal replacement therapy (CRRT) initiation according to AKI risk and patient fluid accumulation in pediatric (3 months to 18 years) and young populations (18 to 25 years).
A comparison of pre-FT2 and post-FT2 showed that after T2 implementation, time to CRRT initiation was two days shorter, ≥15% pre-CRRT fluid accumulation was lower, with shorter lengths of stay after CRRT discontinuation and total ICU. Patients presented higher survival rates in the TF2 era. In conclusion, this assessment can produce durable reductions in pediatric CRRT patient morbidity.
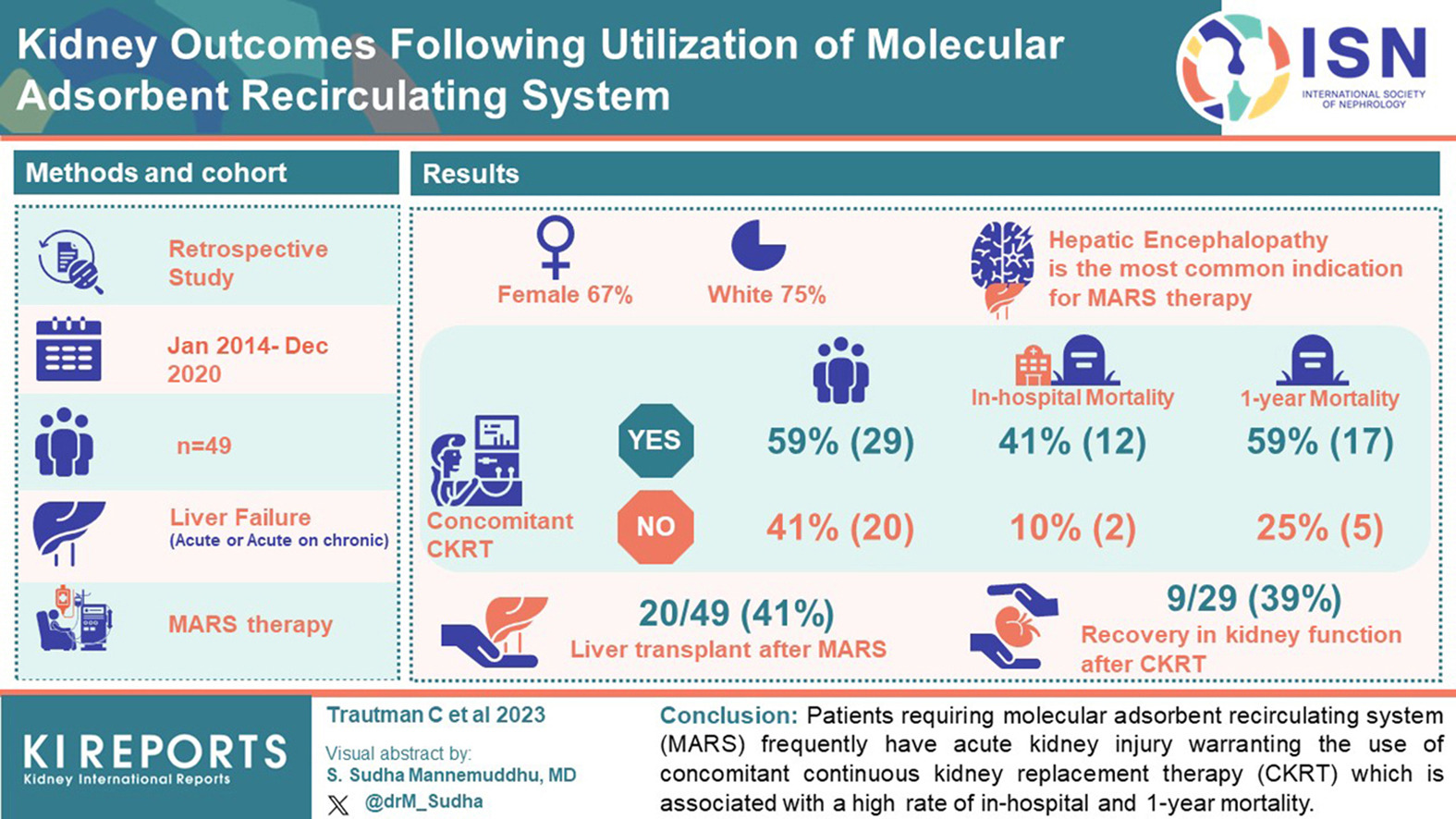
How often do patients with fulminant hepatic failure requiring Molecular Adsorbent Recirculating System (MARS) develop acute kidney injury (AKI)? Would AKI and the concomitant use of continuous kidney replacement therapy CRRT be related to worse outcomes?
In this retrospective study by Trautman et al., 59% of the total patients who received MARS required concomitant CRRT, and 41% initiated it simultaneously.
Patients requiring CRRT presented a higher in-hospital mortality (RR 4.15, 95% CI 1.04 to 16.52, P= 0.044) and one-year mortality (RR 2.92, 95% CI 1.08 to 7.94, P= 0.035). Only 39% of patients recovered kidney function before hospital discharge.
